Introduction:

Osteoarthritis (OA) is the leading cause of disability worldwide (Liu et al. 2022). In the UK, 1 in 10 adults show symptoms and are clinically diagnosed with it with the knee being the most commonly affected joint (Swain et al. 2020). Knee OA is defined as a degenerative disorder of the knee joint primarily caused by the loss of articular cartilage over some time (Haq et al. 2003). It is characterised by the symptom of pain which often worsens on performing an activity (Hsu and Siwiec 2022). The elderly population especially over 65 years of age shows a higher prevalence (Mora et al. 2018). Although the condition is attributed to loss of the cartilage and adjacent joint degeneration it is influenced by multiple other factors like trauma, weight, genetics, age, and mechanical overloading (Heidari 2011). As a result of which the treatment interventions are multifactorial.
As per the National Institute for Health and Care Excellence (NICE) guidelines the physiotherapeutic management of knee OA includes therapeutic exercises, weight loss, manual therapy, acupuncture, and the use of electrotherapeutic devices. Even though land-based therapeutic exercise is a well-established method to relieve the symptoms and improve physical function (Dantas et al. 2021), it might cause an increase in pain at the beginning of the exercise regimen as per the NICE guidelines. The evidence also suggests that weight-bearing exercise aggravates symptoms in these patients which are seen as hydrarthrosis after exercise in these patients (Lund et al. 2008). As obesity is associated with a majority of the population affected with knee OA, the load on the knee joint is further increased (Bliddal et al. 2014). Hydrotherapy is an effective treatment option for such painful conditions (Tapani Pöyhönen et al. 2001, Fransen 2014). The properties of water like buoyancy reduce the load on the joint whereas the temperature and pressure of the water help to reduce swelling and enhance circulation (Biscarini and Giuliano Giorgio Cerulli 2007). However, if hydrotherapy is the most efficient and better treatment option for this condition is still debatable. Hence, this report aims to document evidence for the efficacy of hydrotherapy in reducing pain and improving function in individuals with knee OA and to support that with a treatment protocol.
Search Strategy:
A search was conducted on Scopus, Ovid (MEDLINE, AMED, and Embase), Cinahl, and Pubmed using the search terms mentioned in Table 1. Synonyms and conceptual variants of these terms were searched using the Boolean operator 'OR' and these terms were combined and mismatched together using the Boolean operator 'AND'. Back chaining of the articles was done through their references. The search was restricted from the year 2008 to the current year for clinical relevance. Both gender studies were included, and there was no age barrier for the population as OA being a degenerative disease was studied only in the elderly. Systematic reviews were excluded from the search as they did not provide a detailed description of the intervention protocol. Other participants and study-specific inclusion and exclusion criteria are listed in Table 2. The final shortlisted 5 articles were appraised using the appropriate Critical Appraisal Skills Program (CASP) checklist for randomized control trial (RCT) and Specialist Unit for Review Evidence (SURE) checklist for non-randomized control experimental study.
Table 1: Search terms
1 (Pathology) | 2 (Intervention) |
Knee osteoarthritis ‘OR’ knee osteoarthrosis ‘OR’ knee OA ‘OR’ OA of the knee ‘OR’ degenerative joint disease
| Hydrotherapy ‘OR’ Aqua therapy ‘OR’ aquatic exercise ‘OR’ water exercise ‘OR’ pool-based exercise ‘OR’ aquatic physiotherapy
|
1 and 2 were combined using the Boolean logic ‘AND’ |
Table 2: Inclusion and exclusion criteria
Inclusion Criteria | Exclusion Criteria |
• Published between 2008-2023 • Studies including both male and female population • Includes participants with knee osteoarthritis • Studies that included a protocol of exercise in water • Studies that assessed pain as their primary outcome measure • English language studies | • Studies which included participants who underwent any knee surgery • Studies which included osteoarthritis of any other joint • Aqua therapy studies which did not involve exercising in water • Studies using different minerals in water for spa therapy or balneotherapy • Studies assessing only aquatic cycling • Systematic Reviews |
Outcome Measures:
The pain was the parameter used in the papers as their primary outcome to measure the effectiveness of the intervention. Visual Analog Scale (VAS) was used by the majority of articles to measure pain (Lund et al. 2008, Silva et al. 2008, Taglietti et al. 2018, Sekome and Maddocks 2019). Silva et al. (2008) also used Lequesne Index for OA for pain and discomfort in the knee as a secondary outcome measure. Taglietti et al. (2018) also evaluated pain as a component of Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) along with VAS. Wang et al. (2011) used Knee Injury and Osteoarthritis Outcome Score (KOOS) for pain. VAS has good test-retest reliability and is valid to measure knee pain and produces lesser errors when compared to other pain rating scales (Alghadir et al. 2018). WOMAC and KOOS are both self-reported measures and both of them have shown good validity and reliability for knee conditions. (White and Master 2016). Lequesne Index for OA is a psychometric evaluation questionnaire for OA and there's no strong evidence about its reliability and validity in the general population. Some studies also measured several other factors like function, strength, mobility, range of motion, and depression which will not be addressed for the given intervention in this paper.
Results Overview:
All studies except Lund et al. (2008) concluded that hydrotherapy was an effective treatment in improving pain in individuals with knee OA (Silva et al. 2008, Taglietti et al. 2018, Sekome and Maddocks 2019, Wang et al. 2011). Although most of the studies except Sekome and Maddocks (2019) were randomised control trials they had different control groups. Only Taglietti et al. 2018 concluded that hydrotherapy was better at treating knee OA patients than the control group which was given only patient education. Other three studies (Lund et al. 2008, Silva et al. 2008, Wang et al. 2011) compared hydrotherapy with land-based exercise. Lund et al. 2008 and Wang et al. 2011 had a control group with no treatment as well, these studies concluded that hydrotherapy was more efficient than the control groups but did not show any additional benefits to land-based exercise in reducing pain. Lastly, Lund et al. 2008 stated although improvement in pain was seen only in land-based exercise group, water-based exercises showed fewer adverse effects.
Treatment Protocols:
Although treatment protocols varied from paper to paper, they also had several similarities. Beginning with components of water, the temperature of the water was one important factor considered by all studies. On average the temperature varied between 30-34 degrees Celsius with Wang et al. (2011) having the lowest temperature of 30 degrees, followed by Silva et al. (2008) and Taglietti et al. (2018) at 32 degrees, and Lund et al. (2008) and Sekome and Maddocks (2019) at 33.5 and 34 degrees respectively. Maintaining the water temperature similar to the body temperature helps to regulate homeostasis, especially in the older population which participated in the intervention, besides the thermal properties of warm water also has beneficial effects on other systems of the body like the cardiorespiratory system, cognitive and musculoskeletal system (An et al. 2019). Another component of water mentioned was the depth of the pool, 1.2 meters was the depth demonstrated by two studies (Silva et al. 2008 and Taglietti et al. 2018). Sekome and Maddocks 2019 mentioned the depth to be at the Anterior Superior Iliac Spine (ASIS) height of the participants. Although, there is no strong evidence of the effect of the depth of water on humans but studies in animals have demonstrated that greater muscle activation is required to perform an activity in deeper waters. This is because the off-loading of the body weight is influenced by the depth of water (Torres-Ronda and Alcázar 2014).
The next parameter to be considered is the frequency of treatment, most of the papers conducted the intervention twice a week (Lund et al. 2008, Taglietti et al. 2018, Sekome and Maddocks 2019). Only Silva et al. (2008) and Wang et al. (2011) had a greater frequency of three sessions per week. It is also noteworthy that only these two studies had a longer duration of intervention, 12 weeks for Wang et al. (2011) and 18 weeks for Silva et al. (2008). The other three studies had a shorter duration of intervention with 8 weeks each (Lund et al. 2008, Taglietti et al. 2018) and 4 weeks for Sekome and Maddocks 2019. All sessions in all the papers were around 50 minutes (Lund et al. 2008, Silva et al. 2008) to 60 minutes long (Wang et al. 2011, Taglietti et al. 2018, Sekome and Maddocks 2019).
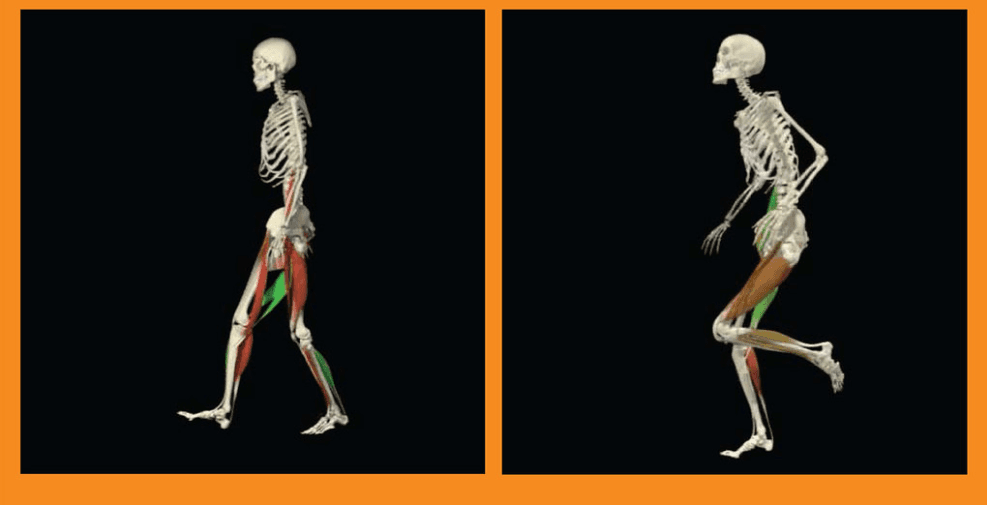
The intervention protocol included various types of exercises, all of them except Silva et al. (2008) started with 5-10 minutes of warm-up and ended with 5-10 minutes of cool down. All the studies included lower limb strengthening exercises in different forms. Taglietti et al. (2018) included isometric exercise and dynamic exercise with elastic bands while Silva et al. (2008) used pelvis floaters for the same. Silva et al. (2008) also conducted isotonic strengthening exercises and progressed the resistance over the weeks. Sekome and Maddocks 2019 also relied on dynamic single and double-legged strengthening exercises underwater. Wang et al. (2011) included lower body training exercises in water without any added resistance. Lund et al. (2008) used the principle of manual resistance applied by the physiotherapist along with components of aerobic resistance in their study. On average, the number of repetitions was 10-15 for the exercise as specified by Wang et al. (2011). Stretching was the next common form of exercise followed by most of the studies except for Sekome and Maddocks (2019). The large muscle groups stretched in the majority of the study were the quadriceps, gluteus, adductors, and abductors of the hip, triceps surae, and hamstrings. (Taglietti et al. 2018, Lund et al. 2008, Silva et al. 2008). Aerobic exercise was the next exercise performed by three out of five studies, Taglietti et al. (2018) and Lund et al. (2008) performed stationary aquatic running as a form of aquatic exercise while Wang et al. (2011) instructed to perform paced walk moves. Balance training was the next type of intervention included in two studies, while Taglietti et al. (2018) paired it with proprioception training, Wang et al. (2011) trained participants for balance and coordination together. Lastly, gait training which is an important treatment for knee OA was only performed by Silva et al. (2008).
Quality:
The quality of the papers demonstrating the efficacy of hydrotherapy is as debatable as the results. Although all participants who participated in the study went through a screening to be eligible to be a part of the study the participants in the study by Wang et al. (2011) were recruited from the local community and sports center, unlike all other studies where the participants were recruited either from an outpatient department or Primary Health care Unit. This creates a selection bias in the participant population (Eldridge et al. 2009).
Another important population factor that might cause a bias is the age of the participants, the participants in Silva et al. (2008) study are comparatively younger than the participants of all other studies. Third and the last population bias seen is the gender-based bias, over 80% of the population in all studies is female. This might have created a bias in any other condition but as knee OA is more commonly seen in females (Bartley et al. 2016, Mora et al. 2018) it will be considered as a benefit or confounder of the intervention (Hicks 2009).
The outcome measure of pain in the form of VAS, WOMAC, and KOOS has shown very controversial results. Taglietti et al. (2018) reported a greater decrease in pain through aquatic exercise on both VAS and WOMAC but it was statistically significant only on WOMAC. This was attributed to the baseline state of the participants stating greater the baseline pain, the better the improvement in VAS (Tubach 2005). This might be the reason greater improvement of pain was seen in participants of the Silva et al. study who had higher baseline scores taken from pain experienced from the previous week, this might have led to a detection bias in these studies (Mohammad Ali Mansournia et al. 2017). Similarly, the use of KOOS instead of VAS by Wang et al. (2011) might have reduced the specificity of pain.
All studies except Sekome and Maddocks (2019) were randomised control trials. Randomisation of the participants was compromised due to inappropriate methods in Lund et al. (2008) and Silva et al. (2008) study which may create a bias in the study (Torgerson and Roberts 1999). As a result of which the allocation sequence could not be concealed from the participants in these studies. Power calculation and precision estimation were carried out for all studies. All studies were single-blinded studies as the assessor measuring the baseline measurement and post-intervention measurement was unaware of the participant's group. Although blinding the participants after disclosing the treatment intervention at first was impossible, blinding the investigators from the aim and objective of the research could have helped reduce the risk of bias (Portney and Watkins 2014).
Baseline characteristics between groups varied in Lund et al. (2008) study where the weight of the land-based exercise group was 13.5 kg lower than the aquatic group even after randomisation, this might have created a bias as weight loss has been associated with a reduction in pain (Christensen et al. 2006). Considering the differences in the group, the control group in the study by Taglietti et al. (2018) was given only patient education and guidelines for a home exercise program while the intervention group was given additional treatment in the form of patellar mobilization and massage along with the aquatic physiotherapy which might have created a risk of bias.
There was a high number of dropouts in all studies. In all studies, there were higher dropouts from the control group when compared to the intervention group. In the study by Lund et al. (2008), there was a high dropout of 11% from the land-based exercise group and 44% reported adverse effects from the same group. Intention to treat analysis was demonstrated in all studies except Wang et al. (2011) which might have affected their analysis causing an attrition bias (Mohammad Ali Mansournia et al. 2017). Higher compliance of participants to hydrotherapy intervention was observed in all studies was observed and possible reasons for it could be lesser discomfort and drive to not grab upon the opportunity to be a part of such a unique intervention in a public setting.
Lastly, the study by Sekome and Maddocks 2019 was a non randomised experimental study, the sample size power calculation was done but the sample size was very small to gather high-quality evidence which increased the bias risk in this study (Hicks 2009). The intervention duration was the shortest with only 4 weeks and had no follow-up, a longitudinal follow-up study might have demonstrated a deeper long-term impact of the intervention.
Conclusion:
This process of literature review aimed to assess the efficacy of hydrotherapy for reducing pain in knee osteoarthritis. The evidence to support this is still very scarce and has other confounding factors like the involvement of other joints or surgical processes, a discrepancy in the type of hydrotherapy, and female gender-biased studies. As a result, only poor to moderate-quality of evidence was developed through this literature. However, the majority of the literature has supported the hypothesis of hydrotherapy being an effective treatment for pain reduction but they failed to prove that it was the best option available. When compared to different groups of comparators it was significantly more efficient than no treatment or patient education but when compared to land-based physiotherapy there was no significant difference. Nevertheless, not undermining the potential benefits of lesser adverse effects and greater patient compliance towards hydrotherapy, it is an efficient alternative treatment option for patients with knee OA who demonstrate difficulty or disinterest in undergoing land-based treatment.
References:
Alghadir, A.H., Anwer, S., Iqbal, A. and Iqbal, Z.A. 2018. Test–retest reliability, validity, and minimum detectable change of visual analog, numerical rating, and verbal rating scales for measurement of osteoarthritic knee pain. J Pain Res. Volume 11, pp. 851–856. doi: 10.2147/JPR.S158847
An, J.-Y., Lee, I. and Yi, Y. 2019. The Thermal Effects of Water Immersion on Health Outcomes: An Integrative Review. Int J Environ Res Public Health. 16(7), pp. 1280–1280. doi: 10.3390/ijerph16071280
Bartley, E.J., King, C.D., Sibille, K.T., Cruz‐Almeida, Y., Riley, III, J.L., Glover, T.L. et al., 2016, ‘Enhanced pain sensitivity among individuals with symptomatic knee osteoarthritis: Potential sex differences in central sensitization’, Arthritis Care & Research 68(4), 472–480. https://doi.org/10.1002/acr.22712
Biscarini A, Cerulli G. Modeling of the knee joint load in rehabilitative knee extension exercises under water. J Biomech. 2006;17:1–11. doi: 10.1016/j.jbiomech.2005.12.018
Christensen, R., Else Marie Bartels, Astrup, A. and Henning Bliddal 2006. Effect of weight reduction in obese patients diagnosed with knee osteoarthritis: a systematic review and meta-analysis. Ann Rheum Dis. 66(4), pp. 433–439. doi: 10.1136/ard.2006.065904
Eldridge, S., Kerry, S. and Torgerson, D.J. 2009. Bias in identifying and recruiting participants in cluster randomised trials: what can be done? BMJ 339(oct09 1), pp. b4006–b4006. doi: https://doi.org/10.1136/bmj.b4006.
Fransen M, McConnell S, Bell M. Therapeutic exercise for people with osteoarthritis of the hip or knee: a systematic review. J Rheumatol. 2002;29:1737–1745.
Haq, I., Murphy, E. and Dacre, J. 2003. Osteoarthritis. BMJ Journals 79(933), pp. 377–383. Doi: 10.1136/pmj.79.933.377 Available at: https://pmj.bmj.com/content/79/933/377 [Accessed: 30 May 2023].
Heidari, B. 2011. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Caspian journal of internal medicine 2(2), pp. 205–12. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3766936/ [Accessed: 30 May 2023].
Henning Bliddal, Leeds, A.R. and Christensen, R. 2014. Osteoarthritis, obesity and weight loss: evidence, hypotheses and horizons – a scoping review. Obes Rev. 15(7), pp. 578–586. doi: 10.1111/obr.12173
Hicks, C. M. 2009. Research methods for clinical therapists: applied project design and analysis. Churchill Livingstone.
Hsu, H. and Siwiec, R.M. 2022. Knee Osteoarthritis. In: StatPearls [Internet]. Available at: https://www.ncbi.nlm.nih.gov/books/NBK507884/ [Accessed: 20 May 2023].
Kganetso Sekome and Maddocks, S. 2019. The short-term effects of hydrotherapy on pain and self-perceived functional status in individuals living with osteoarthritis of the knee joint. S Afr J Physiother. 75(1): 476. doi: 10.4102/sajp.v75i1.476
Liu, M., Jin, F., Yao, X. and Zhu, Z. 2022. Disease burden of osteoarthritis of the knee and hip due to a high body mass index in China and the USA: 1990–2019 findings from the global burden of disease study 2019. BMC Musculoskeletal Disorders 23(1). https://doi.org/10.1186/s12891-022-05027-z
Lucas Ogura Dantas, Salvini, T.F. and McAlindon, T.E. 2021. Knee osteoarthritis: key treatments and implications for physical therapy. Braz J Phys Ther. 25(2), pp. 135–146. doi: 10.1016/j.bjpt.2020.08.004
Luciana Rodrigues Silva, Valim, V., Maria, A., Oliveira, L.M., Myamoto, S., Jones, A. and Natour, J. 2008. Hydrotherapy Versus Conventional Land-Based Exercise for the Management of Patients With Osteoarthritis of the Knee: A Randomized Clinical Trial. Phys Ther. 88(1), pp. 12–21. doi:10.2522/ptj.20060040
Lund, H. et al. 2008. A randomized controlled trial of aquatic and land-based exercise in patients with knee osteoarthritis. J Rehabil Med. 40(2), pp. 137–144. doi: 10.2340/16501977-0134
Mohammad Ali Mansournia, Higgins, J.P.T., Sterne, J.A.C. and Hernán, M.A. 2017. Biases in Randomized Trials. Epidemiology. 28(1), pp. 54–59. doi: 10.1097/EDE.0000000000000564
Mora, J., Przkora, R. and Yenisel Cruz-Almeida 2018. Knee osteoarthritis: pathophysiology and current treatment modalities. J pain Res. Volume 11, pp. 2189–2196. doi: 10.2147/JPR.S154002
Portney, L. G. and Watkins, M. P. 2014. Foundations of clinical research : applications to practice. 3rd Pearson New International Edition ed. Harlow: Pearson.
Swain, S., Aliya Sarmanova, Mallen, C.D., Kuo, C.-F., Coupland, C., Doherty, M. and Zhang, W. 2020. Trends in incidence and prevalence of osteoarthritis in the United Kingdom: findings from the Clinical Practice Research Datalink (CPRD). Osteoarthritis and Cartilage 28(6), pp. 792–801. https://doi.org/10.1016/j.joca.2020.03.004
Taglietti, M. et al. 2018. Effectiveness of aquatic exercises compared to patient-education on health status in individuals with knee osteoarthritis: a randomized controlled trial. Clin Rehabil. 32(6), pp. 766–776. doi: 10.1177/0269215517754240
Tapani P, Kari LK, Heikki K, et al. Neuromuscular function during therapeutic knee exercise under water and on dry land. Arch Phys Med Rehabil. 2001;82: 1146 –1152 doi: 10.1053/apmr.2001.25073
Torgerson, D.J. and Roberts, C. 1999. Understanding controlled trials: Randomisation methods: concealment. BMJ 319(7206), pp. 375–376. doi: 10.1136/bmj.319.7206.375
Torres-Ronda, L. and Alcázar, del 2014. The Properties of Water and their Applications for Training. J Hum Kinet. 44(1), pp. 237–248. doi: 10.2478/hukin-2014-0129
Tsae Jyy Wang, Shu Yen Lee, Liang, S.-Y., Heng Hsin Tung, Wu, S. and Lin, Y. 2011. Comparing the efficacy of aquatic exercises and land-based exercises for patients with knee osteoarthritis. 20(17-18), JClin Nurs. pp. 2609–2622. doi: 10.1111/j.1365-2702.2010.03675.x.
Tubach, F. 2005. Evaluation of clinically relevant changes in patient reported outcomes in knee and hip osteoarthritis: the minimal clinically important improvement. Ann Rheum Dis. 64(1), pp. 29–33. doi: 10.1136/ard.2004.022905.
Vitger, A., Bruhn-Rasmussen, T., Eja Oppenlænder Pedersen, Lene Høeg Fuglsang-Damgaard and Harrison, A.P. 2021. The impact of water depth and speed on muscle fiber activation of healthy dogs walking in a water treadmill. Acta Vet Scan 63(1). https://doi.org/10.1186/s13028-021-00612-z
White, D.K. and Master, H. 2016. Patient-Reported Measures of Physical Function in Knee Osteoarthritis. 42(2), Rheum Dis Clin North Am. pp. 239–252. doi: 10.1016/j.rdc.2016.01.005