Introduction:
Low back pain (LBP) is the prime cause of years lost to disability worldwide (Wu et al. 2020). As per the National Institute of Health and Care Excellence (NICE) guidelines 3-4 % of adults below 45 years and 5-7 % above 45 years are affected by LBP in the UK. LBP is a health condition with pain as a leading complaint and not a pathology in itself and it can be widely classified as a specific and non-specific type (Maher et al. 2017). Discogenic back pain is a distinct type of LBP that accounts for 26-42% of patients (Peng 2013) and affects young as well as elderly individuals (Hironori Hyodo et al. 2005). It is caused by the degeneration of intervertebral disc (IVD) without any herniation, anatomical deformity, or other specific causes of pain and disability (Fujii et al. 2019).
Although LBP has multiple causes IVD degeneration is a primary cause (Mohd et al. 2022) and excessive mechanical loading accelerates the process of degeneration as it disturbs the structure of the disc and further leads to precipitation of a cell-mediated response and cascade of disruption (Michael and Roughley 2006). Forward bending of the trunk has been associated to increase mechanical loads on the lumbar spine, these loads are further increased by adding on weights while bending (Takahashi et al. 2006). Hence, this paper will focus on the pathology of discogenic LBP caused by IVD degeneration and how it links to a mechanically loading action of forward bending of the trunk.
Pathology:
The process of disc degeneration is usually described as an age-related process (Wu 2017) although, instances where the signs of degeneration are observed in young population are not uncommon (Berg et al. 2020). Michael and Roughley (2006) stated that a disc should be termed degenerated only when it demonstrates structural failure along with advanced signs of aging. This latter part of the definition differentiates the degenerated disc from the early degeneration or injured disc. Disc degeneration is defined as an aberrant, cell-mediated response to progressive structural failure (Michael and Roughley 2006). Whereas, early degenerative changes seen in the young population are accelerated age-related changes in which the structure of the disc is not much impacted. Even though this definition explains the difference of the degenerative changes seen in early and later stages of age. Degenerative changes of the spine on imaging are common in many asymptomatic individuals as well (Brinjikji et al. 2014). Therefore, the main factor that distinguishes degenerated disc from a physiologically aging disc is the symptom of pain (Michael and Roughley 2006). The paper by Michael and Roughley (2006) further explained the mechanism of pain stating the highest amount of stress of a degenerated disc is concentrated in the annulus fibrosus hence the pain sensitization is functionally most significant at the annulus. This is because the posterior annulus and the adjacent longitudinal ligament have an autonomic and somatic mixed nerve supply by the sinuvertebral nerve which is nociceptive (Nikolai Bogduk 1985). The nociceptive nerves usually only penetrate the outermost 1 to 3 millimetres of the annulus but there has been evidence of them reaching anteriorly towards the nucleus of a painful and disrupted disc making them susceptible of carrying pain from the entire disc (Freemont et al. 1997, Palmgren et al. 1999). This similar type and density of nerve innervation were observed in the bony endplate as well (Fagan et al. 2003). The basivertebral nerve supplies the subchondral bone in the endplate which can be responsible for the transfer of pain, more research is necessary on this topic. (Lotz et al. 2013). Although endplate fracture is usually seen during high-intensity compressive forces on the vertebrae that are more prevalent in endplate driven disc degeneration (Michael and Dolan 2012).
These findings were in accordance to Peng (2013), attempted to differentiate between the composition and structure of painful discs from non-painful degenerative discs. Structural changes were seen in the nucleus pulposus as well as the annulus fibrosus of a degenerated disc. To understand the results of the study it is important to understand the histological changes in a degenerated disc described by Wu (2017), into three stages: the early stage is when clefts and tears start occurring in the nucleus and inner annulus. This is followed by the proliferation of the chondrocyte which produces a matrix around the structural defect. The next stage is when the clefts extend to the outer annulus and are filled with granular material. Differentiation of fibroblast of the outer annulus into chondrocyte-like cells where the granulation is completed. In the late-stage collagen content and cross-linkage increase, there is no anatomical demarcation possible and the entire disc becomes fibrotic. The characteristic difference described by Peng (2013) in a painful pathological disc was the inflammatory vascular granulation tissue formation was till the nucleus with neuronal innervation along the clefts and tears in the posterior annulus. This formation was absent in the asymptomatic degenerative disc as a result of which pain could not be transmitted as vascularization and innervation only existed until the outermost layers of the annulus.
Peng (2013) highlighted another mechanism of pain through IVD degeneration which was the higher presence of some growth factors like fibroblast growth factor, tissue growth factor β1, and connective tissue growth factor in degenerative discs than in normal discs. These growth factors are required to act on the IVD for their dedifferentiation and proliferation along with the synthesis of extracellular matrix and signal transmission. This evidence was supported by Fujii et al. (2019), who attributed pain in a degenerated disc to disturbance of normal catabolic and anabolic activities (Risbud and Shapiro 2014) along with IVD cells producing increased levels of proinflammatory cytokines that are known to be nociceptive and noxious triggers (Johnson et al. 2017). This was further supported by the evidence that substances like nitric oxide, leukotrienes, prostaglandin E, and lactic acid which are considered nociceptive are increased in IVD degeneration (Ito and Creemers 2013). The strong presence of proliferating cell nuclear antigens in painful discs also supported Fujii et al. (2019) hypothesis of these factors being the main cause of painful disc fibrosis and degeneration.
Discussion:
The process of degeneration is negatively influenced by the daily loading of the spine as it prevents the regeneration of the tissue and leads to further structural defects (Wu 2017). Mechanical stimulation of the outer posterior annulus and endplate of the degenerative disc has been associated with back pain in several pain provocation studies (Kuslich et al. 2023). This is because the discogenic pain from the disc can be detected either from the annulus or from the endplate, classifying the discogenic pain into 'annulus driven' or 'endplate driven' (Michael and Dolan 2012). This same paper by Michael and Dolan (2012) associated substantial forward bending components with annulus-driven degeneration of the disc, usually seen in the lower lumbar spine as the posterior annulus is relatively thinner in these regions. This leads to the formation of radial fissures due to annulus lamellae rupture and migration of the nucleus towards the periphery due to repetitive mechanical loading (Adams and Hutton 1985). Forward flexion aggravates this because bending stretches and weakens the annulus of the side away even more that it is injured before the vertebral endplate can be affected. Additionally, if the stresses on the annulus are remarkably high it often causes disc prolapses (Michael and Dolan 2012). This is because of the unequal distribution of mechanical load in the disc causing structural disruption and making the degenerative disc painful and sensitized (Michael and Roughley 2006).
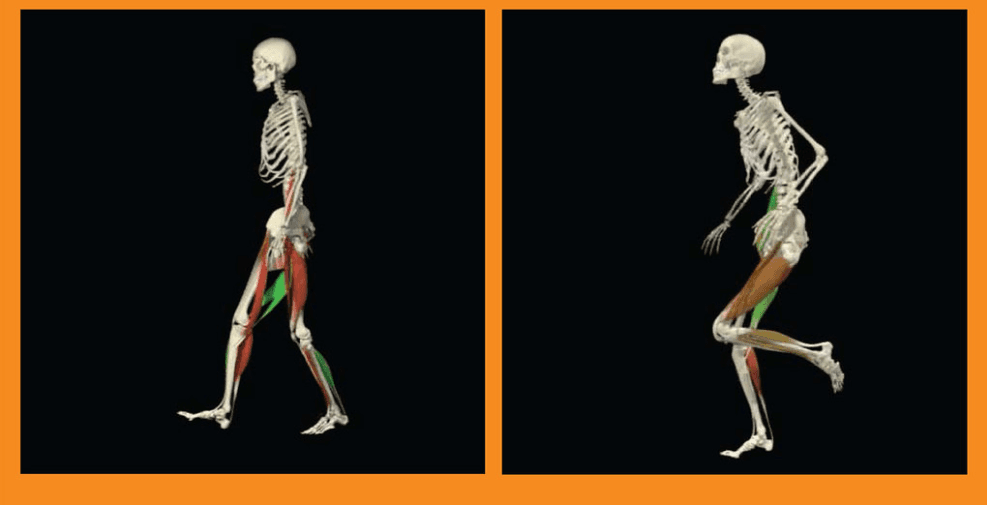
Takahashi et al. (2006) conducted a biomechanical study on the mechanical load on the lumbar spine during forward bending in which they measured the intradiscal pressure, electromyogram activities, and motion analysis of the trunk and surrounding muscles in participants during forward bending with and without lifting a weight. The results indicated that the load on the lumbar spine increased proportionally with the increase trunk tilt while forward bending. The load further increased with increased bending along with external weights as well. The electromyographic activity of the back extensors namely erector spinae kept on increasing with increased loads and forward bending while there was no activity seen in the anterior rectus abdominis muscles.
Iman Shojaei et al. (2018) conducted a case-control design to study the differences in mechanical load on the lower back in non-specific LBP females and healthy females. While considering the biomechanics, patients with LBP did not show any change in trunk range rotation but demonstrated decreased trunk angular acceleration while performing the bending forward and returning to normal tasks. Within the same study, they observed that the patients with LBP demonstrated a larger pelvic rotation and decreased lumbar spine movement during free trunk bending and movement and smaller peak thorax rotation was also observed. This was in line with the findings of Thomas and France (2008) where lumbar flexion was associated with a high level of fear of bending forward in patients with LBP but this fear was not demonstrated in any other parts like the thoracic spine or hip movements. The author suggests that in those patients there was no general tendency of avoidance of movement but a specific restriction of lumbar spine. Iman Shojaei et al. (2018) described this significantly reduced motion at the lumbar spine as an overprotective mechanism by the neuromuscular system in patients to prevent the posterior components of the painful spine from overstretching.
In addition, the difference in the pelvic rotation between the patients and the healthy individuals was more prominent in the age group of 40-50 years whereas the other two groups 50-60 and 60-70 did not show significant differences Iman Shojaei et al. (2018). This might indicate a need for shearing demand which might be a task only demonstrated by the 40–50-year age group. Similar variations in the LBP intensity were demonstrated in a study conducted by Lunde et al. (2019), association of forward bending at work with LBP intensity in construction and healthcare workers was studied. While the study did not show any association in construction workers there was an association seen between ≥30° forward bending at work and a change in the LBP intensity whereas there was no association between exposure to ≥60° at work in healthcare workers. This indicates that the association between LBP and forward bending may be affected by various factors such as the type of task performed, gender, and occupation.
Conclusion:
Even though, discogenic LBP might present itself as an acute or non-specific type of LBP it has a distinct specific pain pathology. IVD degeneration is the primary cause of discogenic LBP and as per the existing evidence, there are two mechanisms of production and transmission of pain. The first is the tissue pathology mechanism where the process of degeneration leads to the process of granulation and innervation in both the nucleus pulposus and annulus fibrosus in a painful and disrupted disc. Another is the biochemical mechanism where the presence of certain growth factors in higher quantities leads to a cascade of disruption.
Although, forward bending is considered as a mechanically loading activity for the spine there is limited literature describing the link between forward bending and discogenic LBP specifically. Forward bending affects the already weakened posterior annulus by unequal distribution of loads and in extreme cases may lead to prolapse or endplate fractures. Lumbar spine movement during forward bending in LBP patients is limited due to fear and as a protective mechanism. Movements at other joints like the thorax, hip, and pelvis have shown contradictory opinions and need further study. The influence of forward bending in LBP also depends on various other factors like the task performed, gender, occupation, duration of bending, angle of tilting, and amount of load carried. While planning the physiotherapeutic interventions for patients with LBP these factors should be taken into consideration.
References:
Adams, M.A. and Hutton, W.C. 1985. Gradual Disc Prolapse. Spine 10(6), pp. 524–531. doi: 10.1097/00007632-198507000-00006.
Berg, A.J., Ahmadje, U., Jayanna, H.H., Trégouët, P., Sanville, P. and Kapoor, V. 2020. The prevalence of lumbar disc degeneration in symptomatic younger patients: A study of MRI scans. Journal of Clinical Orthopaedics and Trauma 11(5), pp. 932–936. doi: 10.1016/j.jcot.2020.07.021
Brinjikji, W. et al. 2014. Systematic Literature Review of Imaging Features of Spinal Degeneration in Asymptomatic Populations. American Journal of Neuroradiology 36(4), pp. 811–816. doi: 10.3174/ajnr.A4173
Buckwalter, J.A. 1995. Aging and Degeneration of the Human Intervertebral Disc. Spine 20(11), pp. 1307–1314. doi: 10.1097/00007632-199506000-00022
Fagan, A.J., Moore, R.B., Barrie Vernon Roberts, Blumbergs, P.C. and Fraser, R.J. 2003. ISSLS Prize Winner: The Innervation of the Intervertebral Disc: A Quantitative Analysis. Spine 28(23), pp. 2570–2576. doi: 10.1097/01.BRS.0000096942.29660.B1
Freemont, A.J., Peacock, T.E., Philippe Goupille, Hoyland, J.A., O'Brien, J.T. and Malcolm 1997. Nerve ingrowth into diseased intervertebral disc in chronic back pain. 350(9072), pp. 178–181. doi: 10.1016/s0140-6736(97)02135-1.
Fujii, K. et al. 2019. Discogenic Back Pain: Literature Review of Definition, Diagnosis, and Treatment. JBMR plus 3(5), pp. e10180–e10180. doi: 10.1002/jbm4.10180
Hironori Hyodo, Sato, T., Sasaki, H. and Tanaka, Y. 2005. Discogenic pain in acute nonspecific low-back pain. European Spine Journal 14(6), pp. 573–577. doi: 10.1007/s00586-004-0844-8
Iman Shojaei, Salt, E., Hooker, Q.L. and Babak Bazrgari 2018. Mechanical demands on the lower back in patients with non-chronic low back pain during a symmetric lowering and lifting task. J Biomech. 70, pp. 255–261. doi: 10.1016/j.jbiomech.2017.06.032.
Ito, K. and Creemers, L.B. 2013. Mechanisms of Intervertebral Disk Degeneration/Injury and Pain: A Review. World Journal of Stem Cells 3(3), pp. 145–151. doi: 10.1055/s-0033-1347300.
Johnson, Z.I., Doolittle, A.C., Snuggs J, Shapiro, I.M., Le, C.L. and Risbud, M.V. 2017. TNF-α promotes nuclear enrichment of the transcription factor TonEBP/NFAT5 to selectively control inflammatory but not osmoregulatory responses in nucleus pulposus cells. J Biol Chem 292(42), pp. 17561–17575. doi: 10.1074/jbc.M117.790378.
Kuslich SD;Ulstrom CL;Michael CJ 2023. The tissue origin of low back pain and sciatica: a report of pain response to tissue stimulation during operations on the lumbar spine using local anesthesia. The Orthopedic clinics of North America 22(2):181-7. Available at: https://pubmed.ncbi.nlm.nih.gov/1826546/ [Accessed: 13 May 2023].
Lotz, J.C., Fields, A.J. and Liebenberg, E.C. 2013. The Role of the Vertebral End Plate in Low Back Pain. Global Spine J 3(3), pp. 153–163. doi:10.1055/s-0033-1347298
Lunde, L.-K., Koch, M., Merkus, S.L., Stein Knardahl, Morten Wærsted and Kaj Bo Veiersted 2019. Associations of objectively measured forward bending at work with low-back pain intensity: a 2-year follow-up of construction and healthcare workers. Occup Environ Med. 76(9), pp. 660–667. doi: 10.1136/oemed-2019-105861
Maher, C.G., Underwood, M. and Buchbinder, R. 2017. Non-specific low back pain. The Lancet 389(10070), pp. 736–747. doi: 10.1016/S0140-6736(16)30970-9. Epub 2016 Oct 11.
Michael and Dolan, P. 2012. Intervertebral disc degeneration: evidence for two distinct phenotypes. Journal of Anatomy 221(6), pp. 497–506. doi: 10.1111/j.1469-7580.2012.01551.x
Michael and Roughley, P.J. 2006. What is Intervertebral Disc Degeneration, and What Causes It? Spine 31(18), pp. 2151–2161. doi: 10.1097/01.brs.0000231761.73859.2c
Mohd, L., Seong Lin Teoh, Huda, N. and Sabarul Afian Mokhtar 2022. Discogenic Low Back Pain: Anatomy, Pathophysiology and Treatments of Intervertebral Disc Degeneration. International Journal of Molecular Sciences 24(1), pp. 208–208. doi: 10.3390/ijms24010208
Nikolai Bogduk 1985. The Innervation of the Vertebral Column. 31(3), pp. 89–94. doi.org/10.1016/S0004-9514(14)60626-7 Available at: https://www.sciencedirect.com/science/article/pii/S0004951414606267?via%3Dihub [Accessed: 15 May 2023].
Palmgren, Tove MD*; Grönblad, Mats MD*†; Virri, Johanna MSc*‡; Kääpä, Eeva MD, PhD§; Karaharju, Erkki MD, PhD*‡.1999. An Immunohistochemical Study of Nerve Structures in the Anulus Fibrosus of Human Normal Lumbar Intervertebral Discs. Spine. 24(20):p 2075
Peng, B.-G. 2013. Pathophysiology, diagnosis, and treatment of discogenic low back pain. World journal of orthopedics 4(2), pp. 42–42. doi: 10.5312/wjo.v4.i2.42
Risbud, M.V. and Shapiro, I.M. 2014. Role of cytokines in intervertebral disc degeneration: pain and disc content. Nat Rev Rheumatol 10(1), pp. 44–56. doi: 10.1038/nrrheum.2013.160.
Takahashi, I., Kikuchi, S., Sato, K. and Sato, N. 2006. Mechanical Load of the Lumbar Spine During Forward Bending Motion of the Trunk–A Biomechanical Study. Spine 31(1), pp. 18–23. doi: 10.1097/01.brs.0000192636.69129.fb.
Thomas, J.S. and France, C.R. 2008. The relationship between pain-related fear and lumbar flexion during natural recovery from low back pain. European Spine Journal 17(1), pp. 97–103. doi: 10.1007/s00586-007-0532-6
Vo, N. et al. 2016. Molecular mechanisms of biological aging in intervertebral discs. 34(8), pp. 1289–1306. J Orthop Res doi: 10.1002/jor.23195.
Wu, A., March, L., Zheng, X., Huang, J., Wang, X., Zhao, J., Blyth, F.M., Smith, E., Buchbinder, R. and Hoy, D. (2020). Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Annals of Translational Medicine, [online] 8(6), pp.299–299. doi:org/10.21037/atm.2020.02.175.
Wu, Q. 2017. Intervertebral Disc Aging, Degeneration, and Associated Potential Molecular Mechanisms. Journal of Head Neck & Spine Surgery 1(4). doi: 10.19080/JHNSS.2017.01.555569