 Discovering your baby has clubfoot can feel overwhelming, but effective treatments are available. With proper early intervention, most children go on to run, jump, and play sports without any limitations. Learn about proven treatment methods and how to support your child's development.If you've just discovered your baby has clubfoot, you're probably feeling overwhelmed with questions. Can clubfoot be corrected? What causes clubfoot in babies? How do you fix clubbed feet effectively?
Discovering your baby has clubfoot can feel overwhelming, but effective treatments are available. With proper early intervention, most children go on to run, jump, and play sports without any limitations. Learn about proven treatment methods and how to support your child's development.If you've just discovered your baby has clubfoot, you're probably feeling overwhelmed with questions. Can clubfoot be corrected? What causes clubfoot in babies? How do you fix clubbed feet effectively?
The good news is that clubfoot is highly treatable when caught early. With proper intervention, most children go on to live completely normal, active lives. Let's explore everything you need to know about this common condition.
What Is Clubfoot and How Does It Present?
Clubfoot, medically known as Congenital Talipes Equinovarus, is a complex foot deformity present at birth. It's characterised by four key structural abnormalities that cause the foot to point downward and inward in a rigid position[1].
The condition affects multiple planes of motion and often comes with underdeveloped calf muscles and tendon abnormalities. Unlike positional foot anomalies that can be gently corrected, true clubfoot resists passive manipulation and requires professional treatment[2,3,4].
What makes clubfoot different from other pediatric foot conditions like metatarsus adductus (pigeon toes) is its rigidity and involvement of the hindfoot. It's a structural problem that won't resolve on its own, which is why early intervention is crucial.
When Does Clubfoot Appear?
Clubfoot develops during a critical window of foetal development, specifically between the 9th and 14th weeks of pregnancy[6]. This is when your baby's limbs and musculoskeletal system are forming.
Prenatal ultrasound can detect clubfoot in approximately 60-80% of cases, typically around 22 weeks of pregnancy[5]. However, the accuracy depends on factors like foetal position, the severity of the deformity, and the technician's experience.
Some mild cases might not be diagnosed until birth, which is why thorough examination of newborns is so important[6]. Early detection gives you and your medical team the best chance for successful treatment.What Causes Clubfoot in Babies?
Understanding clubfoot baby causes can help ease some of your concerns. Around 80% of cases occur without a known cause (idiopathic), while the remaining 20% are linked to other medical conditions[8,4].
Genetic Factors
Research shows a strong genetic component to clubfoot. Multiple genes are involved in limb development, including PITX1, TBX4, and various HOX genes[9]. If you have a family history of clubfoot, your baby's risk increases significantly.
About 25% of cases show familial patterns, but the condition can skip generations[10]. It's caused by a mix of different genes, which explains why not everyone who carries these genes develops clubfoot.
Developmental Issues
Clubfoot often results from abnormal foetal development during those crucial weeks 9-14 of pregnancy[7]. The condition involves shortened tendons, muscle weakness, and joint malformations that create an imbalance.
These developmental disruptions cause a cascade of structural changes. Neuromuscular imbalances create uneven muscle pulls during bone formation, resulting in the characteristic inward and downward foot deviation.
Environmental Risk Factors
Several maternal and environmental factors can increase clubfoot risk:
Maternal Smoking: Cigarette smoking during pregnancy significantly increases clubfoot risk[11]. Toxic compounds like nicotine and carbon monoxide disrupt normal foetal blood flow and oxygen delivery to developing limbs.
Oligohydramnios: Reduced amniotic fluid creates physical constraints that limit foetal movement[12]. This restricted environment prevents normal musculoskeletal development and joint positioning.
First Pregnancy: First pregnancies show a modest but consistent increased risk for clubfoot[13]. The relatively tighter uterine environment may create increased mechanical constraints on foetal movement.
Non-Surgical Treatment Options: The Gold Standards
The wonderful news is that most clubfoot cases can be successfully treated without surgery. Early intervention is key to achieving the best possible outcomes.
The Ponseti Method
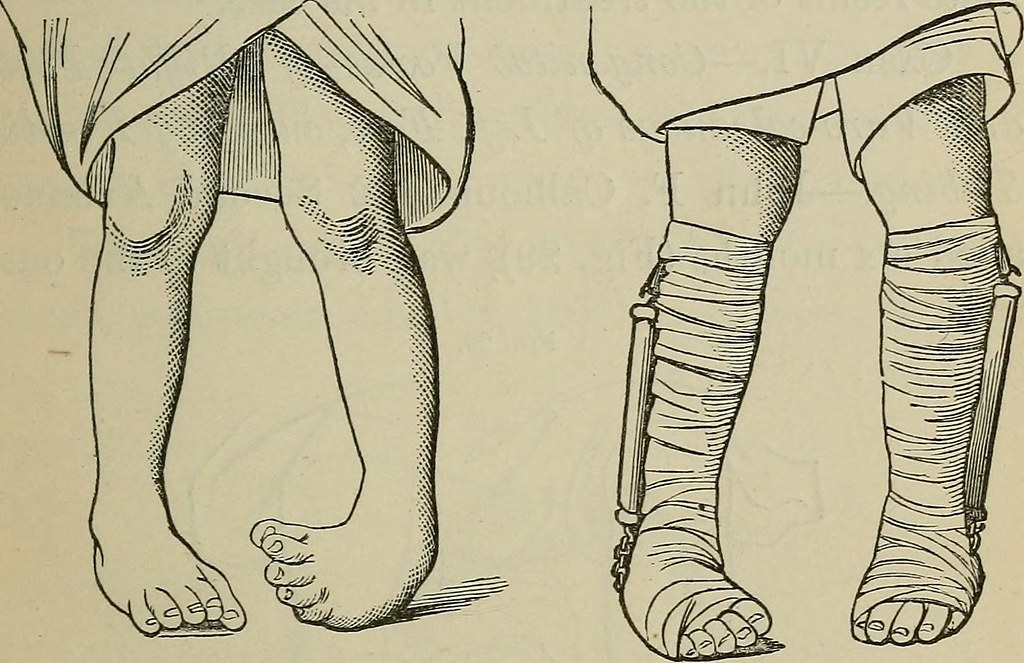
The Ponseti Method is the gold standard for treating clubfoot. Developed by Dr Ignacio Ponseti in the 1960s, this approach involves gentle manipulations and progressive casting.
The process typically includes cutting the Achilles tendon to correct the downward bending of the foot. After casting, your child will wear a foot abduction brace for 23 hours daily for three months, then only during sleep until around age four.
When used correctly, the Ponseti Method achieves full correction in up to 98% of cases[14]. Studies show excellent long-term results, with 78% maintaining good or excellent function even 30 years post-treatment[15].
French Functional Method
The French Method is a conservative technique involving muscle stimulation and nonelastic adhesive strapping. Treatment begins soon after birth and continues intensively for about two months.
This method is ideal for mild clubfoot cases but requires skilled physiotherapists and highly committed parents. Daily treatment and home-based care are critical for success.
While improvement occurs in the first three months, progress is typically slower than the Ponseti method. It works best in contexts with strong physiotherapy infrastructure.
Dynamic Bracing
Dynamic bracing is an emerging technique that offers a modern alternative to traditional rigid braces. The Dobbs Method uses flexible, spring-loaded bars that allow controlled foot motion while maintaining correction[16].
This approach aims to improve comfort and compliance, particularly helpful for children who resist wearing rigid braces. It's most suitable after successful Ponseti correction, especially where brace compliance is a concern.When Surgery Becomes Necessary
Sometimes, despite best efforts with conservative treatment, surgical intervention becomes necessary. This happens when clubfoot doesn't respond to non-surgical methods or when relapses occur.
Soft Tissue Release Procedures
Soft tissue release involves surgical lengthening of tight tendons and ligaments. The posteromedial release (PMR) is the most common approach, addressing all components of the clubfoot deformity.
Surgery is considered when conservative treatment fails after 3-6 months, typically showing minimal improvement after 5-7 cast changes[17]. It's also indicated for severe rigid deformities and neglected cases in older children.
The optimal timing is typically around six months of age[18]. Earlier surgery increases scarring risk, while delayed intervention may lead to permanent bony changes.
Advanced Surgical Options
For older children with relapsed or resistant clubfoot, more extensive procedures may be necessary. Tendon transfers, such as the anterior tibial tendon transfer, correct muscle imbalances by relocating tendons[19].
Osteotomies (bone cuts) become necessary when fixed bony deformities develop, usually in children over five years[20]. These procedures realign the skeletal architecture when bones have become mispositioned.
These invasive procedures are reserved for severe cases where soft tissue procedures alone would be insufficient due to established bony deformity.
Long-Term Care and Monitoring
Successful clubfoot treatment doesn't end with initial correction. Long-term follow-up care is essential to maintain results and support your child's ongoing development.
Bracing Protocol
Following initial correction, rigorous bracing is essential to maintain results. The foot abduction brace should be worn 23 hours daily for the first three months, then during nighttime until age 4-5 years.
Regular monitoring appointments help catch early signs of recurrence. Initially monthly, then quarterly visits allow for immediate intervention rather than waiting for problems to develop.
Exercise and Strengthening
A personalised stretching and strengthening programme becomes increasingly important as your child grows. Gentle stretching exercises typically begin around six months post-correction.
Age-appropriate activities help develop strength and balance. For toddlers, playful "toe grabbing" games strengthen foot muscles whilst making therapy enjoyable.
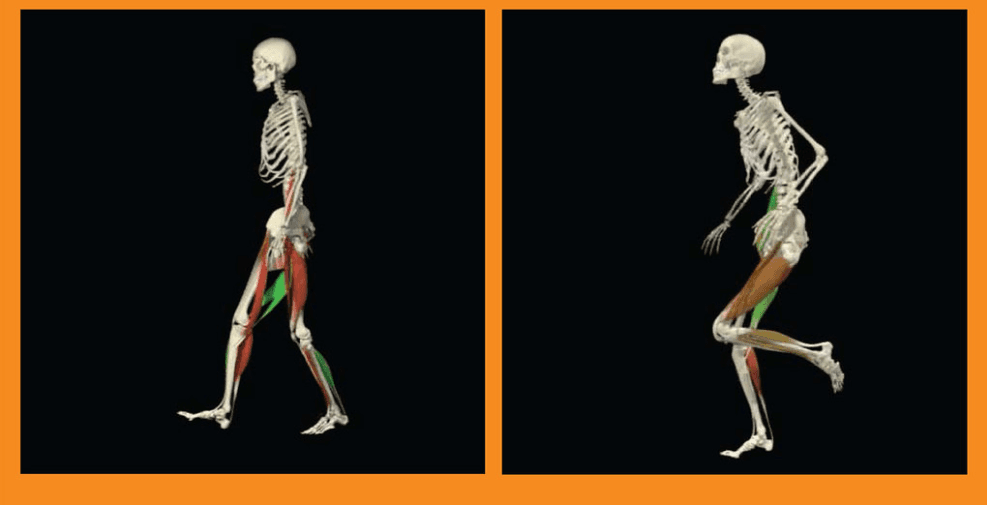
Gait Analysis
Regular gait analysis becomes critical as your child develops more complex movement patterns. Initially, observational assessments during clinic visits are sufficient.
As children reach age 3-4, more structured evaluations help identify subtle compensations that could lead to long-term issues. Video recordings of walking can provide valuable comparative records.
» Find out more about gait abnormalities in children
Gender Differences and Personalised Care
Boys are more frequently affected by clubfoot (approximately 2.5:1 ratio), but treatment response is generally similar between genders[21]. However, girls with idiopathic clubfoot may occasionally have slightly higher chances of relapse[22].
These differences may be influenced by genetic factors affecting musculoskeletal development. While the standard protocol remains the same, individualised care with attention to early signs of relapse is advisable for all children.
Promising Innovations in Clubfoot Care
Exciting developments are improving clubfoot detection and treatment outcomes:
3D Ultrasound Technology: Significantly enhances prenatal detection with 97% sensitivity and 90% specificity for predicting treatment necessity[23].
Machine Learning Algorithms: Show promise for predicting treatment responses and developing personalised protocols[24].
Botulinum Toxin Therapy: Emerging as valuable adjunctive treatment for resistant cases, enabling greater correction through muscle relaxation.[25]
Dynamic Bracing Systems: Modern alternatives to rigid braces that improve comfort and compliance in young children
Supporting Your Family Through Treatment
Remember that clubfoot treatment affects the whole family. Parents often experience significant emotional distress, including anxiety and depression during the treatment process.
Structured psychosocial support programmes can improve treatment compliance and family wellbeing. Don't hesitate to seek support from healthcare professionals, support groups, or counselling services.
Long-term studies show that individuals treated for clubfoot maintain good functional outcomes into adulthood. With proper treatment and follow-up care, your child can expect to live a completely normal, active life.
From First Cast to Final Brace: What Matters Most
Clubfoot is a treatable condition with excellent outcomes when managed properly. Early detection and intervention are crucial for success, but even cases diagnosed later can achieve good results.
Whether your baby's clubfoot requires the Ponseti method, physiotherapy, or surgical intervention, the key is working with experienced healthcare professionals and following through with long-term care plans.
Your dedication to your child's treatment will pay off. With proper care, most children with clubfoot go on to run, jump, play sports, and live completely normal lives without limitations.
A. Barrie and M. A. Varacallo, “Clubfoot,” StatPearls - NCBI Bookshelf, Aug. 07, 2023. Available: https://www.ncbi.nlm.nih.gov/books/NBK551574/
A. I. Gore and J. P. Spencer, “The newborn foot,” AAFP, Feb. 15, 2004. Available: https://www.aafp.org/pubs/afp/issues/2004/0215/p865.html
D. Dibello, V. Di Carlo, G. Colin, E. Barbi, and A. M. C. Galimberti, “What a paediatrician should know about congenital clubfoot,” the Italian Journal of Pediatrics/Italian Journal of Pediatrics, vol. 46, no. 1, Jun. 2020, doi: 10.1186/s13052-020-00842-3. Available: https://doi.org/10.1186/s13052-020-00842-3
Introduction to Clubfoot. (2025, February 16). Physiopedia, . Retrieved 14:48, May 22, 2025 from https://www.physio-pedia.com/index.php?title=Introduction_to_Clubfoot&oldid=366162.
Y.-M. Kim et al., “Improving prenatal diagnosis precision for congenital clubfoot by using Three-Dimensional ultrasonography,” Diagnostics, vol. 14, no. 1, p. 117, Jan. 2024, doi: 10.3390/diagnostics14010117. Available: https://pmc.ncbi.nlm.nih.gov/articles/PMC10795686/
H. Bogers et al., “First trimester physiological development of the fetal foot position using three‐dimensional ultrasound in virtual reality,” Journal of Obstetrics and Gynaecology Research, vol. 45, no. 2, pp. 280–288, Nov. 2018, doi: 10.1111/jog.13862. Available: https://doi.org/10.1111/jog.13862
“Clubfoot Treatment Options | HSS Lerner Children’s Pavilion,” Hospital for Special Surgery. Available: https://www.hss.edu/condition-list_clubfoot.asp
M. Umar, L. Tong, H. Jin, T. Terebessy, and D. Chen, “Genetics, epidemiology and management of clubfoot and related disorders,” Genes & Diseases, p. 101690, May 2025, doi: 10.1016/j.gendis.2025.101690. Available: https://doi.org/10.1016/j.gendis.2025.101690
R. Panza, F. Albano, A. Casto, C. Del Vecchio, N. Laforgia, and D. Dibello, “Incidence and prevalence of congenital clubfoot in Apulia: a regional model for future prospective national studies,” the Italian Journal of Pediatrics/Italian Journal of Pediatrics, vol. 49, no. 1, Nov. 2023, doi: 10.1186/s13052-023-01559-9. Available: https://doi.org/10.1186/s13052-023-01559-9
K. C. Dickinson, R. E. Meyer, and J. Kotch, “Maternal smoking and the risk for clubfoot in infants,” Birth Defects Research, vol. 82, no. 2, pp. 86–91, Nov. 2007, doi: 10.1002/bdra.20417. Available: https://doi.org/10.1002/bdra.20417
“Limb deformations in oligohydramnios sequence: effects of gestational age and duration of oligohydramnios,” PubMed, Oct. 29, 1999. Available: https://pubmed.ncbi.nlm.nih.gov/10508984/
“Idiopathic congenital talipes equinovarus in Wisconsin newborns: incidence and associated risk factors,” PubMed, Apr. 01, 2022. Available: https://pubmed.ncbi.nlm.nih.gov/35442577/
J. A. Morcuende, L. A. Dolan, F. R. Dietz, and I. V. Ponseti, “Radical reduction in the rate of extensive corrective surgery for Clubfoot using the Ponseti method,” PEDIATRICS, vol. 113, no. 2, pp. 376–380, Feb. 2004, doi: 10.1542/peds.113.2.376. Available: https://pubmed.ncbi.nlm.nih.gov/14754952/
J. A. Morcuende, L. A. Dolan, F. R. Dietz, and I. V. Ponseti, “Radical reduction in the rate of extensive corrective surgery for Clubfoot using the Ponseti method,” PEDIATRICS, vol. 113, no. 2, pp. 376–380, Feb. 2004, doi: 10.1542/peds.113.2.376. Available: https://publications.aap.org/pediatrics/article-abstract/113/2/376/66875/Radical-Reduction-in-the-Rate-of-Extensive?redirectedFrom=fulltext
R. C. Chen, J. E. Gordon, S. J. Luhmann, P. L. Schoenecker, and M. B. Dobbs, “A new dynamic foot abduction orthosis for clubfoot treatment,” Journal of Pediatric Orthopaedics, vol. 27, no. 5, pp. 522–528, Jul. 2007, doi: 10.1097/bpo.0b013e318070cc19. Available: https://pubmed.ncbi.nlm.nih.gov/17585260/
J. Abraham, J. C. Wall, M. Diab, and C. Beaver, “Ponseti Casting vs. Soft Tissue Release for the Initial Treatment of Non-idiopathic Clubfoot,” Frontiers in Surgery, vol. 8, May 2021, doi: 10.3389/fsurg.2021.668334. Available: https://doi.org/10.3389/fsurg.2021.668334
K. N. Kuo and P. A. Smith, “Correcting residual deformity following Clubfoot releases,” Clinical Orthopaedics and Related Research, vol. 467, no. 5, pp. 1326–1333, Dec. 2008, doi: 10.1007/s11999-008-0664-y. Available: https://journals.lww.com/clinorthop/abstract/2009/05000/correcting_residual_deformity_following_clubfoot.30.aspx
G. H. Thompson, H. A. Hoyen, and T. Barthel, “Tibialis Anterior Tendon Transfer after Clubfoot Surgery,” Clinical Orthopaedics and Related Research, vol. 467, no. 5, pp. 1306–1313, Feb. 2009, doi: 10.1007/s11999-009-0757-2. Available: https://pmc.ncbi.nlm.nih.gov/articles/PMC2664443/?utm_source
H. M. El-Tayeby, “The neglected clubfoot: A salvage procedure,” The Journal of Foot & Ankle Surgery, vol. 37, no. 6, pp. 501–509, Nov. 1998, doi: 10.1016/s1067-2516(98)80027-6. Available: https://pubmed.ncbi.nlm.nih.gov/9879045/?utm_source
M. K. Saini, A. Vijay, M. Gupta, and H. Harshwardhan, “Management of clubfoot by ponseti method: A prospective study,” Journal of Orthopaedics and Allied Sciences, vol. 5, no. 1, p. 27, Jan. 2017, doi: 10.4103/joas.joas_33_16. Available: https://doi.org/10.4103/joas.joas_33_16
R. Y. Goldstein, D. A. Seehausen, A. Chu, D. A. Sala, and W. B. Lehman, “Predicting the need for surgical intervention in patients with idiopathic clubfoot,” Journal of Pediatric Orthopaedics, vol. 35, no. 4, pp. 395–402, Jul. 2014, doi: 10.1097/bpo.0000000000000282. Available: https://pubmed.ncbi.nlm.nih.gov/25075887/
Y.-M. Kim et al., “Improving prenatal diagnosis precision for congenital clubfoot by using Three-Dimensional ultrasonography,” Diagnostics, vol. 14, no. 1, p. 117, Jan. 2024, doi: 10.3390/diagnostics14010117. Available: https://pubmed.ncbi.nlm.nih.gov/38201425/
C. Schaibley, B. Torres-Izquierdo, and P. Hosseinzadeh, “Outcomes of Ponseti method for the treatment of clubfeet in children with arthrogryposis,” Journal of Pediatric Orthopaedics, vol. 44, no. 8, pp. 508–512, Apr. 2024, doi: 10.1097/bpo.0000000000002715. Available: https://pubmed.ncbi.nlm.nih.gov/38689454/?utm_source
C. M. Alvarez, J. G. Wright, H. Chhina, A. Howren, and P. Law, “Botulinum toxin type A versus placebo for idiopathic clubfoot,” Journal of Bone and Joint Surgery, vol. 100, no. 18, pp. 1589–1596, Sep. 2018, doi: 10.2106/jbjs.17.01652. Available: https://pubmed.ncbi.nlm.nih.gov/30234623/?utm_source